Funny Names for a Chest Drainage Tube
Note: This guideline is currently under review.
- Introduction
- Aim
- Definition of Terms
- Indications for Insertion
- Insertion
- Set Up
- Management
- Removal of chest drain
- Complications and Troubleshooting
- Family Centred Care
- Companion Documents
- References
- Evidence Table
Introduction
Chest drains also known as under water sealed drains (UWSD) are inserted to allow draining of the pleural spaces of air, blood or fluid, allowing expansion of the lungs and restoration of negative pressure in the thoracic cavity. The underwater seal also prevents backflow of air or fluid into the pleural cavity. Appropriate chest drain management is required to maintain respiratory function and haemodynamic stability. Chest drains may be placed routinely in theatre, PICU and NICU; or in the emergency department and ward areas in emergency situations.
Some cardiac surgical patients will have Redivac drains inserted, these are different from UWSD. Please refer to redivac guideline http://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Pleural_and_mediastinal_drain_management_after_cardiothoracic_surgery/
Aim
To describe safe and competent management of (UWSD) chest drains by the health care team.
Definition of terms
Chylothorax: Collection of lymph fluid in the pleural space
Haemothorax: Collection of blood in the pleural space
Pneumothorax: Collection of air in the pleural space
Tension Pneumothorax: One way valve effect which allows air to enter the pleural space, but not leave. Air builds up and forces a mediastinal shift. This leads to decreased venous return to the heart and lung collapse/compression causing acute life-threatening respiratory and cardiovascular compromise. Ventilated patients are particularly high risk due to the positive pressure forcing more air into the pleural space. Tension pneumothorax can result in rapid clinical deterioration and is an emergency situation
Pleural effusion: Exudate or transudate in the pleural space
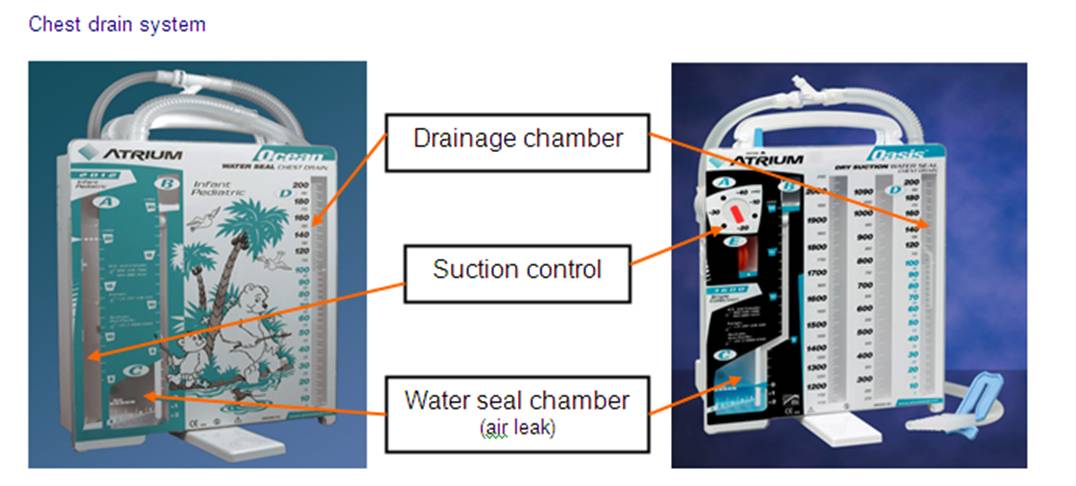
Under Water Seal Drain (UWSD): Drainage system of 3 chambers consisting of a water seal, suction control and drainage collection chamber. UWSD are designed to allow air or fluid to be removed from the pleural cavity, while also preventing backflow of air or fluid into the pleural space
Flutter valve (e.g. Pneumostat, Heimlich valve): One way valve system that is small and portable for transport or ambulant patients. Allows air or fluid to drain, but not to backflow into pleural cavity.
Indications for Insertion of a Chest Drain
- Post operatively e.g. cardiac surgery, thoracotomy
- Pneumothorax
- Haemothorax
- Chylothorax
- Pleural effusions
Insertion of a Chest Drain
See the Chest Drain (Intercostal Catheter) Insertion Clinical Practice Guideline.
RCH access only: See Aseptic Technique Policy and Procedure
Chest Drain Set Up
- Perform Hand Hygiene
- Open drain packaging in an aseptic, 'no-touch' manner
- Prepare drain as per manufacturer's instructions
- Pass sterile end of tubing to Doctor inserting drain when they are ready
- Apply suction to drain if ordered
- Secure drain and tubing and patient
- Secure all connections with cable ties
- Perform hand hygiene
Management
Chest drains should not be clamped unless ordered by medical staff
There is a risk of the patient developing a tension pneumothorax if a drain is clamped while an air leak is present
Start of shift checks
- Patient assessment
- Chest drain assessment
- Equipment
- Ensure that Chest Drain is recorded in the EMR under the LDA flowsheet
- Other considerations e.g physiotherapy referral
Patient Assessment
- Vital signs
- PICU and NICU patients should be on continuous monitoring
- HR, SpO2, BP, RR
- Routine observations:
- For ward areas:
- On insertion of chest drain monitor patient observations of HR, SpO2, BP, RR:
- 15 minutely for 1 hour
- 1 hourly for 4 hours
- Includes HR, SpO2, BP, RR, Respiratory Effort and temperature
- 1-4 hourly as indicated by patient condition
- Observations to be recorded in the Observation Flowsheet on EMR
- On insertion of chest drain monitor patient observations of HR, SpO2, BP, RR:
Pain
- Chest tubes are painful as the parietal pleura is very sensitive. Patients require regular pain relief for comfort, and to allow them to complete physiotherapy or mobilis
- Pain assessment should be conducted frequently and documented in EMR
Drain insertion site
- Observe for signs of infection and inflammation and document findings in EMR
- Check dressing is clean and intact
- Observe sutures remain intact and secure (particularly long term drains where sutures may erode over time)
Assessment of chest tube and system tubing should occur at the beginning of the shift and every hour throughout the shift
UWSD Unit and tubing
- Never lift drain above chest level
- The unit and all tubing should be below patient's chest level to facilitate drainage
- Tubing should have no kinks or obstructions that may inhibit drainage
- Ensure all connections between chest tubes and drainage unit are tight and secure
- Connections should have cable ties in place
- Tubing should be anchored to the patient's skin to prevent pulling of the drain
- In PICU and NICU tubing should also be secured to patient bed to prevent accidental removal
- Ensure the unit is securely positioned on its stand or hanging on the bed
- Ensure the water seal is maintained at 2cm at all times
Suction
- Suction is not always required, and may lead to tissue trauma and prolongation of an air leak in some patients
- If suction is required orders should be written by medical staff
- Atrium Oasis- The wall suction should be set at >80mmHg or higher
- Atrium Ocean- Suction needs to be titrated so that the fluid in suction chamber is gently bubbling
- Suction on the Drainage unit should be set to the prescribed level
- -5 cmH20 is commonly used for neonates
- -10 cmH20 to -20 cmH20 is usually used by convention for children
- -5 cmH20 is commonly used for neonates
- To check suction:
- Atrium Oasis UWSD:
- The bellows should be out to the '?' mark @ 20 cmH20
- Any visible expansion of the bellows is adequate for suction <20 cmH20
- If the bellows deflate, check the wall suction is still working, set to > 80mmHg and that the suction tubing is not kinked
- Atrium Ocean UWSD:
- The water level in the suction chamber should be at prescribed level and gentle bubbling should be observe
- The level may drop due to evaporation or over-vigorous bubbling, if this occurs top fluid level up as per manufacturer's instructions
Drainage
- Milking of chest drains is only to be done with written orders from medical staff. Milking drains creates a high negative pressure that can cause pain, tissue trauma and bleeding
- Volume
- Document hourly the amount of fluid in the drainage chamber in the Fluid Balance flowsheet on EMR
- Calculate and document total hourly output if multiple drains
- Calculate and document cumulative total output
- Notify medical staff if there is a sudden increase in amount of drainage
- Greater than 5mls/kg in 1 hour
- Greater than 3mls/kg consistently for 3 hours
- Blocked drains are a major concern for cardiac surgical patients due to the risk of cardiac tamponade
- Notify medical staff if a drain with ongoing loss suddenly stops draining
- If the chamber tips over and blood has spilt into next chamber, simply tip the chamber up to allow blood to flow to original chamber
- Colour and Consistency
- Monitor the colour/type of the drainage. If there is a change eg. Haemoserous to bright red or serous to creamy, notify medical staff.
- Monitor the colour/type of the drainage. If there is a change eg. Haemoserous to bright red or serous to creamy, notify medical staff.
Air Leak (bubbling)
- An air leak will be characterised by intermittent bubbling in the water seal chamber when the patient with a pneumothorax exhales or coughs
- The severity of the leak will be indicated by numerical grading on the UWSD (1-small leak 5-large leak)
- Continuous bubbling of this chamber indicates large air leak between the drain and the patient. Check drain for disconnection, dislodgement and loose connection, and assess patient condition. Notify medical staff immediately if problem cannot be remedied.
- Document on Fluid Balance Flowsheet on EMR
Oscillation (swing)
- The water in the water seal chamber will rise and fall (swing) with respirations. This will diminish as the pneumothorax resolves.
- Watch for unexpected cessation of swing as this may indicate the tube is blocked or kinked
- Cardiac surgical patients may have some of their drains in the mediastinum in which case there will be no swing in the water seal chamber.
- Document on Fluid Balance Flowsheet on EMR
Equipment by the bedside
- Drain Clamps: At least 2 drain clamps per drain
- For use in emergency only e.g. accidental disconnection
- Two suction outlets: One for chest drain and one for airway management
Other Considerations
- Referral to physiotherapist should be made to enhance chest movement and prevent a chest infection
Patient Positioning
- Patients who are ambulant post operatively will have fewer complications and shorter lengths of stay. Consider converting to a portable flutter valve system such as the pneumostat to facilitate this. If chest drain will be required for prolonged period
- If a patient is on strict bed rest or is an infant, regular changes in position should be encouraged to promote drainage, unless clinical condition prevents doing so
Patient Transport
- If the patient needs to be transferred to another department or is ambulant, the suction should be disconnected and left open to air.
- DO NOT CLAMP THE TUBE
- Clamps must not be used on the patient for transport because of the risk of tension pneumothorax
- Ensure the chamber is below the patient's chest level during transport
- Flutter Valve systems (pneumostat, Heimlich) may be used for patient interhospital transfers (e.g. NETS and PETS)
Specimen Collection
Collect drainage specimens for culture through the needless sampling port located by the in line connector.
Equipment Required
- Specimen container
- Alcohol swab
- 10ml syringe
- Dressing pack
- Gloves
- Eye Protection
Procedure:
- Wait for the fluid to collect in a loop of the tubing
- Perform hand hygiene, then don gloves & eye protection
- Clean the sampling port, or for smaller sampling volumes you can use the patient tube, with an alcohol wipe and leave to dry for 20 seconds
- Clamp the tubing above where the fluid has collecte
- Connect a 10ml Luer lock syringe to the sampling port and aspirate the fluid out of the tubing. If using the patient tube clamp the tubing then use a 20 gauge needle with syringe to aspirate specimen.
- Place fluid in sterile specimen container
- Once the syringe is disconnected remove all clamps and kinks
- Perform hand hygiene
Chest Drain Dressings
Dressings should be changed if:
- no longer dry and intact, or signs of infection e.g. redness, swelling, exudate
- Infected drain sites require daily changing, or when wet or soiled
- No evidence for routine dressing change after 3 or 7 days
- This procedure is a risk for accidental drain removal so avoid unnecessary dressing changes
Exact type of dressing may depend on treating medical team
For cardiac surgical patients with drains inserted intraoperatively:
- ensure dressing does not communicate with sternotomy dressing or wound
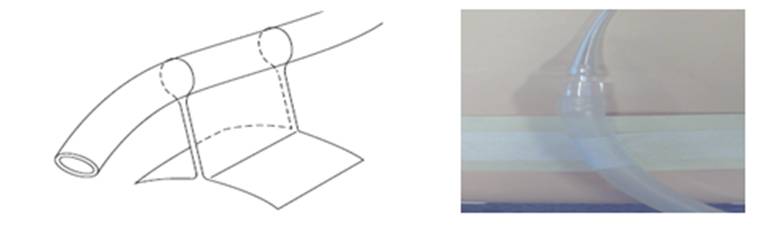
- Sandwich drain between occlusive dressing
- If site oozing dress with split gauze and occlusive dressing
For all other chest drains:
- Sandwich between occlusive dressing
- Allows site visibility and prevents pressure on skin
- If site oozing dress with split gauze and occlusive dressing
Ensure drain is secure
- To prevent it falling out use a 'tag' of tape to secure to skin
- Apply ComfeelTM or similar to protect fragile skin from 'tag' of tape: or,
- Use a securement device such as a grip-lockTM to secure the drains to the skin
Removal of Dressings
- To remove dressing when placed flat against the skin
- Lift corner from the skin and slowly stretch the in dressing in a motion that is parallel to the skin
- Lift corner from the skin and slowly stretch the in dressing in a motion that is parallel to the skin
- To remove semi permeable dressing placed in a sandwich position
- Hold the corners of the dressing on either side of the drain and pull them away from each other; this should create a pocket around the drain
- Peel each of the dressings away from each other until you reach patient skin
- Slowly stretch the rest of the pressing in a motion that is parallel to the patient's skin to remove the rest of the dressing.
Changing the Chamber
- Indications
- The chest drain chamber needs to be replaced when it is ¾ full or when the UWSD system sterility has been compromised eg. Accidental disconnection.
- Equipment Required
- New UWSD
- Dressing pack
- Gloves
- Eye Protection
Procedure
- Perform hand hygiene
- Use personal protective equipment to protect from possible body fluid exposure
- Using an aseptic technique, remove the unit from packaging and place adjacent to old chamber
- Prepare the new UWSD as per manufacturer's directions supplied with drain
- Ensure patients drain is clamped to prevent air being sucked back into chest
- Disconnect old chamber by holding down the clip on the in line connector to pull the tubing away from the chamber.
- Insert the tubing into the new chamber until you hear it click.
- Unclamp the chest drain
- Check drain is back on suction
- Place old chamber into yellow infectious waste bag and tie
- Perform hand hygiene
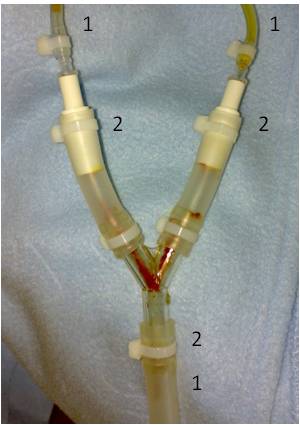
Splitting the UWSD Chambers
- Indications
- When 2 chest drains are connected via a Y-connector into 1 drainage chamber there may be a need to have them split into 2 chambers to determine if 1 drain is draining more than the other
- When 2 chest drains are connected via a Y-connector into 1 drainage chamber there may be a need to have them split into 2 chambers to determine if 1 drain is draining more than the other
- Equipment Required
- New UWSD
- Dressing pack
- Gloves
- Eye Protection
- Chlorhexidine
- Scissors
- Connector
- Cable tie wraps
- Cable tie gun
- New UWSD
Procedure (also see figure below)
- See Aseptic Technique Policy and Procedure
- Perform hand hygiene
- Use personal protective equipment to protect from possible body fluid exposure
- Place newly prepared drainage system in a position adjacent to the old system as set up as per chest drain set up.
- Clamp all tubing
- Cut the tie wraps with the Pliers
- Remove the Y connector and attached tubing
- Clean ends of exposed drains And wait 20 seconds
- Attach drainage system to chest drain
- Repeat with second chamber
- Place tie wraps around connection site and pull to tighten
- Tighten further using Cable tie Gun
- Once secure remove clamps and check for signs suction has returned
Removal of Chest Drains
There must be a written order by medical staff in EMR
Indications
- Absence of an air leak (pneumothorax)
- Drainage diminishes to little or nothing
- No evidence of respiratory compromise
- Chest x-ray showing lung re-expansion
Equipment required
- Dressing trolley with Yellow Infectious waste bag attached
- Dressing pack (sterile towel, sterile gauze)
- Sterile Gloves
- Steristrips
- Suture Cutter
- Band Aids
- Normal Saline
- Clamps
- Eye Protection
- Occlusive dressing
- Sharps container
- Appropriate skin cleaning solution for procedure
- Neonates <1500 grams- Chlorhexidine irrigation solution 0.1% (Blue Solution)
- For all other patients- Aqueous Chlorhexidine 0.15% w/v cetrimide 15% (Yellow Solution)
- Neonates <1500 grams- Chlorhexidine irrigation solution 0.1% (Blue Solution)
Patient preparation
- Ensure Patient is fasted, has been administered adequate pain control, sedation and distraction therapy (see procedural sedation guideline http://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Procedural_Pain_Management/)
- Consider environment i.e. treatment room, privacy screens if in ward area etc
- Heparin infusions for cardiac patients should not be discontinued prior to drain removal
Procedure
- Perform hand hygiene
- Opening dressing pack and add sterile equipment and 0.9% saline
- Don disposable gloves
- Remove all dressings around the area
- Clamp drain tubing
- If there are multiple drains insitu, clamp all drains before removal. Once the required drains are removed, unclamp remaining drains
- Remove disposable gloves, perform hand hygiene and don sterile gloves
- Place sterile towel under tubes
- Clean around catheter insertion site and 1-2cm of the tubing with age appropriate skin cleaning solution
- If purse string present (cardiac patients) unwind in preparation for assistant to tie
- Remove suture securing drain (ensuring purse string suture not cut)
- Instruct patient exhale and hold if they are old enough to cooperate; if not, time removal with exhalation as best as possible.
- Pinching the edges of the skin together, remove the drain using smooth, but fast, continuous traction.
- The assistant pulls purse string suture closed as soon as the drain is removed, tying 2 knots and ensuring the suture is not pulled too tight. Cut tails of suture about 2cm from knot
- If there is no purse string present remove drain and quickly seal hole with occlusive dressing
- Instruct patient to breathe normally again
- Apply occlusive dressing (bandaid for cardiac children) over site
- Remove and discard equipment into a yellow infectious waste bag and tie
- Perform hand hygiene
Post Procedure Care
- Attend to patients comfort and sedation score as per procedural sedation guideline
- CXR should be performed post drain removal
- Patients in PICU may wait until routine daily CXR if clinically well
- Clinical status is the best indicator of reaccumulation of air or fluid. CXR should be performed if patient condition deteriorates
- Monitor vital signs closely (HR, SpO2, RR and BP) on removal and then every hour for 4 hours post removal, and then as per clinical condition
- Document the removal of drain in the LDA flowsheet in EMR
- Remove sutures 5 days post drain removal
- Dressing to remain insitu for 24 hours post removal unless contaminated
- Complications post drain removal include pneumothorax, bleeding and infection of the drain site
Complications and Troubleshooting
Pneumothorax
- Signs and symptoms include: Decreased SpO2, increased WOB, diminished breath sounds, decreased chest movement, complaints of chest pain, tachycardia or bradycardia, hypotension
- Notify medical staff
- Request urgent CXR
- Ensure drain system is intact with no leaks, or blockages such as kinks or clamps
- Prepare for insertion/ repositioning of chest drain
Bleeding at the drain site
- Don gloves
- Apply pressure to insertion site
- Place occlusive dressing over site
- Notify medical staff
- Check Coagulation results
- Check drain chamber to ensure no excessive blood loss
Infection of insertion site
- Notify medical staff
- Swab wound site
- Consider blood cultures
Accidental disconnection of system
- Clamp the drain tubing at the patient end. Clean ends of drain and reconnect. Ensure all connections are cable tied. If a new drainage system is needed cover the exposed patient end of the drain with sterile dressing while new drain is setup. Ensure clamp removed when problem resolved
- Check vital signs
- Alert medical staff
Accidental drain removal
- Apply pressure to the exit site and seal with steri-strips. Place an occlusive dressing over the top
- Check vital signs
- Alert medical staff.
- A VHIMS must be completed by the patient nurse.
Purse string cut or not present
- Small bore drains such as pigtails do not require purse strings. Simply apply an occlusive dressing.
- For large bore drains:
- Pinch or apply pressure to the exit site
- Apply steri-strips to close exit site and cover with an occlusive dressing
- Notify the responsible medical team to review patient and consider need for a suture
- A VHIMS must be completed by the nurse delegated to remove the drain.
Unable to remove chest drain
- If the drain is unable to be removed with reasonable traction being applied, notify the responsible medical team
Retained drain during removal
- If the tube fractures during drain removal and remnants of the tubing is left within the patient contact the treating team
- A chest x-ray should be conducted as soon as possible.
- The patient should be prepared for theatre
- The whole drain unit should be kept in the patient's room until surgical review and will need to be kept for collection to enable quality review.
- The piece of drain tubing that remains in the patient will also be kept once surgically removed to allow for appropriate follow up of the incidents cause.
- A VHIMS must be completed by the nurse delegated to remove the drain.
- Please refer to Surgical Drains (Non Cardiac) guideline http://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Surgical_Drains_(Non_Cardiac)/
& RCH policy http://www.rch.org.au/policy/policies/Surgical_Wounds_-_Procedure_for_Missing_or_Non_Intact_Drains/
Family Centred Care
- Explain purpose of chest drain to family and when it is likely to be removed
- Discuss the need for pain relief for the child to be comfortable enough to move and participate in physiotherapy
Companion Documents
- Chest drain insertion guideline
- Atrium education web site
- Procedural pain management
- http://www.rch.org.au/links/VHIMS/
References
- Charnock, Y and Evans,D. (2001). Nursing management of chest drains: a systematic review. Australian Critical Care. 14(4):156-160
- Curley, M.A. & Moloney-Harmon, P.(2001). Critical care nursing of infants & children. (2nd ed.). Phildelphia: W.B. Saunders Company.
- Durai R; Hoque H; and Davies T. (2010). Managing a chest tube and drainage system. AORN Journal. 91(2):275-280
- Laws, D; Neville, E; & Duffy,J. (2003) BTS guidelines for the insertion of a chest drain. Thorax. 58(suppII):ii53-ii59.
- Newcomb, A; Alphonso N; Norgaard M; Cochrane A; Karl T; Brizard C. (2005) High-vacuum drains rival conventional underwater-seal drains after pediatric heart surgery. European Journal of Cardiothoracic Surgery. 27:395-400
- Pacharn,P; Hellar,D; Kammen,B; Bryce,T; Reddy,M; Baily,R and Brasch,R. (2002). Are chest radiographs routinely necessary following thoracostomy tube removal? Pediatric Radiology. 32:138-142
- Tang, A; Velissaris,T; and Weedon,D. (2002). An evidence based approach to drainage of the pleural cavity: evaluation of best practice. Journal of Evaluation in Clinical Practice. 8(3):333-340
- Van den Boom J; and Battin B. (2007).Chest radiographs after removal of chest drains in neonates: Clinical benefit or common practice? Archives of Disease in Childhood (Neonatal edition). 92:46-48
- http://www.rch.org.au/uploadedFiles/Main/Content/rchcpg/Dressing_Choices.pdf
- http://www.kaleidoscope.org.au/site/content.cfm?page_id=353949¤t_category_code=8337&leca=930
Evidence Table
- Evidence table for Chest Drain Management
Please remember to read the disclaimer
The development of this nursing guideline was coordinated by Daniel Wall and Grace Larson, Rosella PICU, and approved by the Nursing Clinical Effectiveness Committee. Updated February 2016.
Source: https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Chest_drain_management/
0 Response to "Funny Names for a Chest Drainage Tube"
Post a Comment